Macular Edema Following Intravitreal Triamcinolone as an Alternative to Post Cataract Anti-inflammatory Drops
James S. Lewis, MD
Elkins Park, PA
ABSTRACT
To investigate the incidence of macular edema following uncomplicated cataract surgery in which intravitreal triamcinolone is injected in lieu of post-operative topical steroids and NSAIDs.
BACKGROUND
Dropless cataract surgery has been proposed as an alternative to the standard of care. Presently, patients self-administer topical antibiotics, steroids and NSAIDs multiple times a day for one to eight weeks. The impetus for this investigation includes rampant medication non-compliance, excessive branded drug costs, non-physician initiated pharmaceutical substitution, increased generic drug prices, uncertain bioavailability, excess toxicity, erratic formulary coverage policies, and the deliberate and drastic reduction in branded pharmaceutical sampling.
Ophthalmologists, optometrists and office staff have become a virtual sales force for the pharmaceutical industry navigating the drug procurement process. This includes negotiating the compromise between the high cost of drops and patient financial resources, amending the electronic medical record when the doctor’s first choice is rejected, and responding to unpredictable coverage adjudication and other inefficiencies which disrupt our present system.
In an era in which public health optimization vies with individual patient care and physicians are mandated to work more efficiently with fewer resources, responsible health care providers must find an alternative to this untenable system. A cataract procedure without post-operative drops has been the surgeon’s goal for decades.
METHODS AND MATERIALS
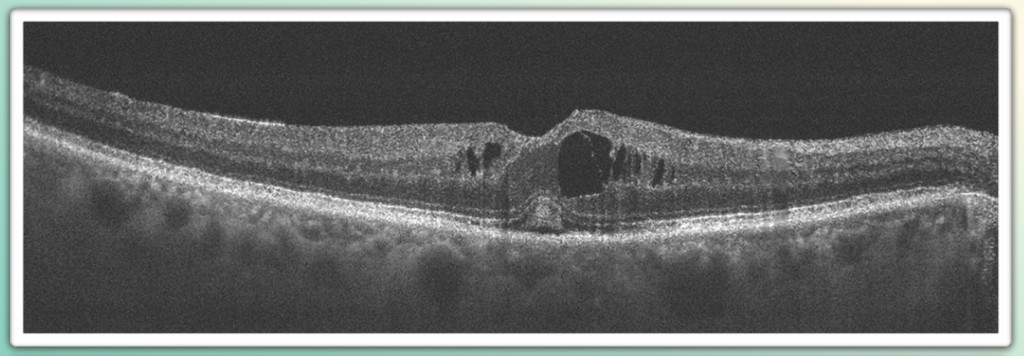
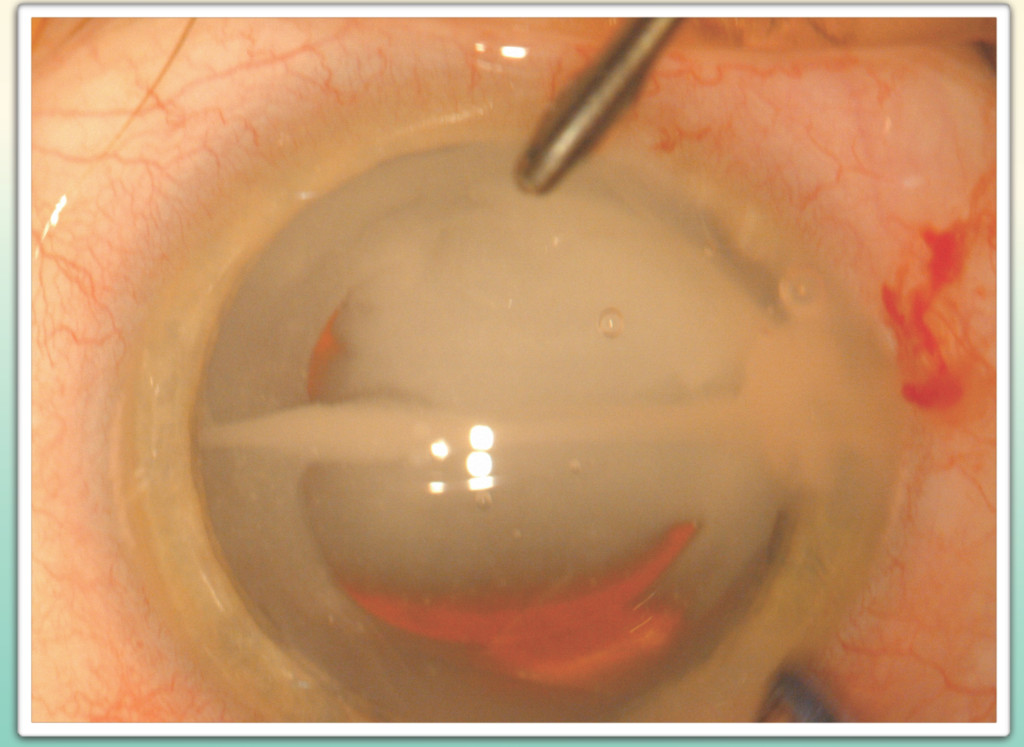
200 consecutive cataract procedures of 129 patients without pre-existing macular pathology from a single surgeon private practice were imaged with retinal OCT pre-operatively and at one day, one week, one month, and two months following uncomplicated surgery. Following intraocular lens implantation and prior to visocelastic removal a transzonular instillation of 0.2cc of a commercially available compounded medication* containing triamcinolone acetonide was performed. The central foveal thickness (CFT) was recorded in all cases at the intervals described above.
RESULTS
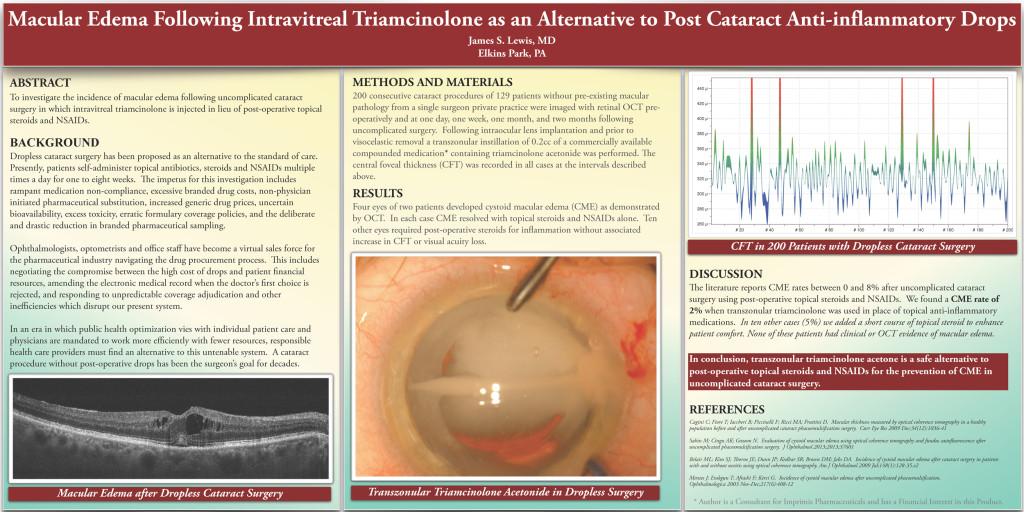
Four eyes of two patients developed cystoid macular edema (CME) as demonstrated by OCT. In each case CME resolved with topical steroids and NSAIDs alone. Ten other eyes required post-operative steroids for inflammation without associated increase in CFT or visual acuity loss.

DISCUSSION
The literature reports CME rates between 0 and 8% after uncomplicated cataract surgery using post-operative topical steroids and NSAIDs. We found a CME rate of 2% when transzonular triamcinolone was used in place of topical anti-inflammatory medications. In ten other cases (5%) we added a short course of topical steroid to enhance patient comfort. None of these patients had clinical or OCT evidence of macular edema.
[su_box title=”CONCLUSION” box_color=”#4A60B1″ radius=”0″]
In conclusion, transzonular triamcinolone acetone is a safe alternative to post-operative topical steroids and NSAIDs for the prevention of CME in uncomplicated cataract surgery.
[/su_box]
REFERENCES
Cagini C; Fiore T; Iaccheri B; Piccinelli F; Ricci MA; Fruttini D. Macular thickness measured by optical coherence tomography in a healthy population before and after uncomplicated cataract phacoemulsification surgery. Curr Eye Res 2009 Dec;34(12):1036-41
Sahin M; Cingu AK; Gozum N. Evaluation of cystoid macular edema using optical coherence tomography and fundus autofluorescence after uncomplicated phacoemulsification surgery. J Ophthalmol 2013;2013:37601
Belair ML; Kim SJ; Thorne JE; Dunn JP; Kedhar SR; Brown DM; Jabs DA. Incidence of cystoid macular edema after cataract surgery in patients with and without uveitis using optical coherence tomography. Am J Ophthalmol 2009 Jul;148(1):128-35.e2
Mentes J; Erakgun T; Afrashi F; Kerci G. Incidence of cystoid macular edema after uncomplicated phacoemulsification. Ophthalmologica 2003 Nov-Dec;217(6):408-12
* Author is a Consultant for Imprimis Pharmaceuticals and has a Financial Interest in this Product.